Acute Lymphoblastic Leukemia (ALL) is a fast-growing form of cancer that affects the blood and bone marrow, primarily impacting children but also diagnosed in adults. Traditional treatments, such as chemotherapy and radiation, have long been the standard, but these methods often come with significant side effects and do not always guarantee long-term remission. In recent years, cell therapy has emerged as a groundbreaking and promising approach to treating ALL, offering hope to patients who may not respond to conventional treatments.
What is Acute Lymphoblastic Leukemia?
ALL is characterized by the overproduction of immature white blood cells (lymphoblasts) in the bone marrow, which crowd out healthy cells and lead to symptoms like fatigue, frequent infections, and easy bruising. If left untreated, ALL can progress rapidly and become life-threatening. While chemotherapy has been effective in achieving remission in many cases, the aggressive nature of ALL means that relapse can occur, especially in high-risk patients.
The Promise of Cell Therapy in Treating ALL
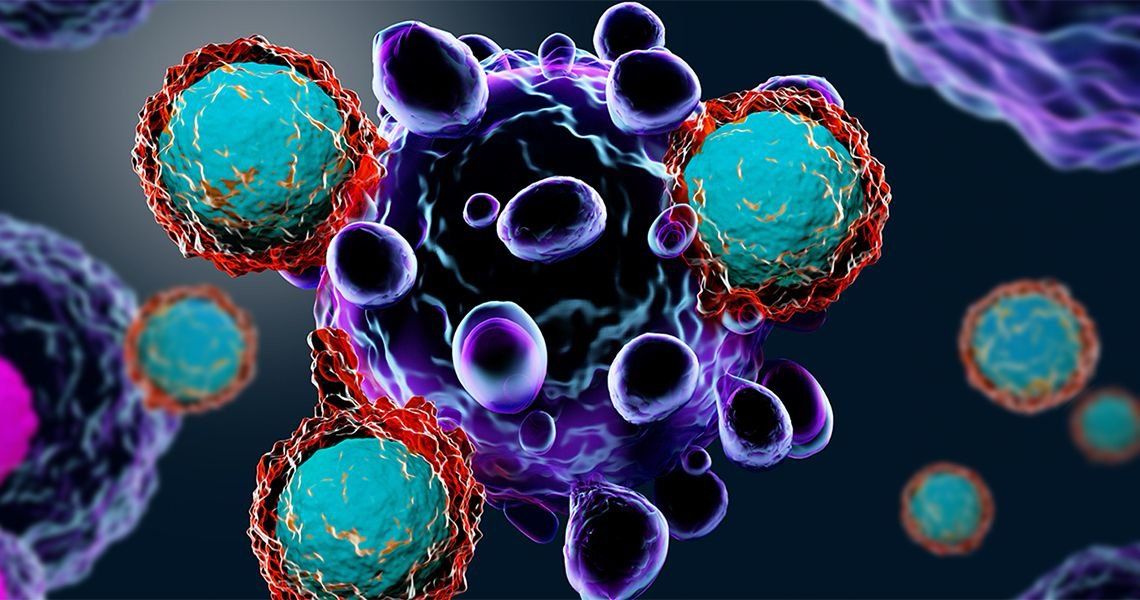
Cell therapy, particularly chimeric antigen receptor T-cell therapy (CAR-T), has revolutionized the treatment landscape for ALL. CAR-T therapy is a type of immunotherapy that uses the patient’s own immune system to fight cancer cells. Here’s how it works:
1. T-Cell Extraction: T-cells, a type of white blood cell that plays a crucial role in immune defense, are collected from the patient’s blood.
2. Genetic Modification: In the lab, these T-cells are genetically modified to produce chimeric antigen receptors (CARs) on their surface. CARs allow the T-cells to recognize and attach to a specific protein, CD19, found on the surface of leukemia cells.
3. T-Cell Infusion: The modified T-cells are multiplied and then infused back into the patient’s bloodstream, where they hunt down and destroy leukemia cells.
How CAR-T Therapy Works Against ALL
CAR-T therapy is particularly effective in treating B-cell acute lymphoblastic leukemia, the most common form of ALL. By targeting the CD19 protein, which is present on nearly all B-cells (both healthy and cancerous), CAR-T cells can precisely attack the leukemia cells while sparing most other tissues. This targeted approach reduces some of the collateral damage typically seen in traditional therapies like chemotherapy, which can harm healthy cells as well.
Studies have shown that CAR-T therapy can induce remission in patients with relapsed or refractory ALL, including those who have not responded to other treatments. In some cases, patients have achieved long-lasting remission, offering a new lease on life for those facing limited options.
The Success of CAR-T Therapy: Real-World Impact
Clinical trials of CAR-T therapy have yielded impressive results, particularly in children and young adults with relapsed or refractory ALL. Some trials have reported remission rates of up to 80% within the first few months of treatment. These results have sparked optimism in the medical community and led to the approval of CAR-T therapies such as Kymriah (tisagenlecleucel) by the U.S. Food and Drug Administration (FDA) for treating pediatric and young adult patients with B-cell ALL.
While CAR-T therapy is not without its challenges—such as managing side effects like cytokine release syndrome (CRS)—its potential to provide long-term remission has made it a game-changer for many ALL patients.
Expanding the Horizons of Cell Therapy
Beyond CAR-T therapy, researchers are exploring other forms of cell-based therapies for treating ALL, including:
• Natural Killer (NK) Cells: NK cells, another component of the immune system, are being studied for their ability to target and kill leukemia cells without the need for genetic modification.
• Stem Cell Transplants: In some cases, patients with ALL may undergo a stem cell transplant (bone marrow transplant) to replace their diseased bone marrow with healthy cells, offering another potential cure for the disease.
The future of cell therapy in ALL treatment is bright, with ongoing research aimed at enhancing the efficacy of CAR-T therapy and reducing its side effects.
Challenges and Future Directions
Despite its success, cell therapy for ALL comes with challenges. The cost of CAR-T therapy is significant, limiting its accessibility for many patients. Additionally, while CAR-T therapy can lead to durable remissions, relapse remains a concern for some patients, especially if leukemia cells lose the CD19 protein that CAR-T cells target.
Researchers are exploring ways to improve the durability of CAR-T responses, such as dual-targeting CAR-T cells, which can recognize more than one protein on leukemia cells, reducing the chances of escape mechanisms. There is also ongoing work to minimize side effects like CRS and neurotoxicity, which can occur when the immune system overreacts to the CAR-T cells.
Conclusion: A New Era in ALL Treatment
Cell therapy, especially CAR-T therapy, has ushered in a new era of hope for patients with acute lymphoblastic leukemia. By harnessing the power of the immune system to specifically target leukemia cells, CAR-T therapy offers a highly effective treatment option for those who have exhausted conventional therapies. As research continues and advances are made, the role of cell therapy in treating ALL will only grow, offering even more patients the chance for long-term remission and a better quality of life.
Sources: