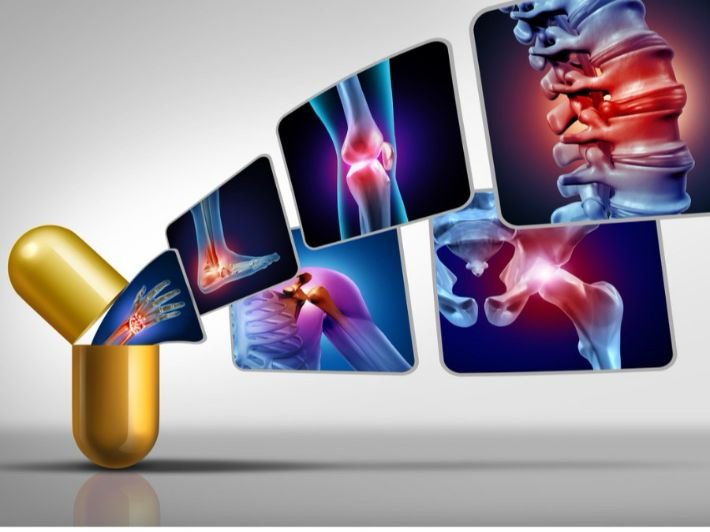
Osteoarthritis, often referred to as “wear-and-tear” arthritis, is a degenerative joint disease that affects millions of people around the world. It occurs when the protective cartilage that cushions the ends of bones wears down over time, leading to pain, stiffness, and decreased joint mobility. Osteoarthritis can affect any joint, but it most commonly impacts the knees, hips, hands, and spine. While there is no cure for osteoarthritis, early diagnosis and effective management can help individuals maintain their quality of life and reduce symptoms. In this article, we will explore the causes, symptoms, treatments, and lifestyle changes that can help those suffering from osteoarthritis.
Understanding Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis and affects more than 30 million adults in the United States alone. It primarily results from the gradual breakdown of cartilage, the flexible tissue that allows joints to move smoothly. As cartilage wears away, bones begin to rub against each other, leading to joint pain, inflammation, and stiffness. Over time, this degeneration can result in loss of joint function and mobility.
Causes and Risk Factors
Several factors can contribute to the development of osteoarthritis, including:
- Aging: The risk of osteoarthritis increases with age, as joint wear and tear accumulate over time. By the age of 65, many individuals show signs of joint degeneration.
- Genetics: A family history of osteoarthritis can increase the likelihood of developing the condition. Certain genetic mutations that affect cartilage production and maintenance can also make individuals more prone to OA.
- Joint Injury: Previous injuries, such as fractures or ligament tears, can accelerate cartilage breakdown and lead to early onset of osteoarthritis.
- Obesity: Carrying excess weight puts added stress on weight-bearing joints, particularly the knees and hips. Over time, this can lead to faster cartilage wear.
- Repetitive Stress: Jobs or activities that require repetitive joint movements, such as manual labor or sports, can lead to increased joint stress and cartilage damage.
- Joint Malalignment: Abnormal joint alignment, whether congenital or the result of injury, can lead to uneven wear on the cartilage.
Symptoms of Osteoarthritis

Osteoarthritis symptoms often develop gradually and worsen over time. Common symptoms include:
- Pain: Joint pain is the hallmark symptom of osteoarthritis. The pain may be worse after physical activity or at the end of the day.
- Stiffness: Stiffness in the affected joints, particularly after periods of inactivity or upon waking up, is common.
- Swelling: Some individuals experience mild swelling in the affected joint due to inflammation.
- Loss of Flexibility: As cartilage wears away, joint movement becomes restricted, leading to reduced flexibility and mobility.
- Grating Sensation: A feeling of grating or cracking may occur when moving the affected joint, indicating that the bones are rubbing against each other.
Diagnosis of Osteoarthritis
Diagnosing osteoarthritis typically involves a combination of physical exams, patient history, and imaging tests. A healthcare provider will assess joint pain, stiffness, and swelling. Imaging techniques such as X-rays or MRI scans can reveal the extent of cartilage loss and joint damage. Additionally, lab tests, including blood tests and joint fluid analysis, may be used to rule out other conditions like rheumatoid arthritis or gout.
Treatment Options for Osteoarthritis
While there is no cure for osteoarthritis, several treatment options can help manage symptoms and improve quality of life. Treatment plans typically focus on reducing pain, maintaining joint function, and preventing further damage. These include:
- Medications:
- Pain Relievers: Over-the-counter pain medications like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help alleviate pain and inflammation.
- Topical Creams: Topical ointments containing NSAIDs or capsaicin can provide localized pain relief when applied to the affected joint.
- Corticosteroid Injections: In some cases, corticosteroid injections into the joint can provide temporary relief from severe pain and inflammation.
- Physical Therapy:
A physical therapist can develop a personalized exercise program to strengthen the muscles surrounding the affected joints, improve flexibility, and enhance joint stability. Regular exercise can help reduce joint pain and improve mobility. - Weight Management:
Losing excess weight can significantly reduce the strain on weight-bearing joints like the knees and hips. Even a small amount of weight loss can lead to substantial improvements in joint pain and function. - Assistive Devices:
The use of braces, canes, or orthotic shoe inserts can help support the affected joints, reduce pain, and prevent further damage by improving joint alignment. - Joint Surgery:
For individuals with severe osteoarthritis who do not respond to other treatments, joint surgery may be an option. Common surgical interventions include:
- Arthroscopy: A minimally invasive procedure used to remove loose cartilage or repair damaged tissues within the joint.
- Joint Replacement Surgery: In cases of advanced osteoarthritis, joint replacement surgery (such as knee or hip replacement) may be necessary to restore mobility and alleviate pain.
Lifestyle Changes to Manage Osteoarthritis
In addition to medical treatments, adopting certain lifestyle changes can help individuals with osteoarthritis manage their symptoms and maintain their quality of life.
- Exercise: Regular low-impact exercise, such as swimming, cycling, or walking, can help strengthen the muscles surrounding the joints, improve flexibility, and reduce joint pain. Stretching exercises are also beneficial in maintaining joint mobility.
- Diet: A healthy, balanced diet can promote joint health and overall well-being. Consuming foods rich in omega-3 fatty acids (found in fish), antioxidants (found in fruits and vegetables), and anti-inflammatory properties can help reduce joint inflammation.
- Heat and Cold Therapy: Applying heat or cold to affected joints can provide relief from pain and stiffness. Heat helps relax muscles and increase blood flow, while cold therapy can reduce inflammation and numb painful areas.
- Stress Management: Chronic pain and mobility limitations can lead to emotional distress. Engaging in stress-relief activities such as yoga, meditation, or deep breathing exercises can improve mental well-being and help individuals cope with the challenges of osteoarthritis.
Preventing Osteoarthritis
While some risk factors for osteoarthritis, such as aging and genetics, are beyond an individual’s control, certain lifestyle choices can help prevent or delay the onset of joint degeneration:
- Maintain a Healthy Weight: Keeping a healthy weight reduces the strain on joints, particularly in the knees and hips, and can delay the progression of osteoarthritis.
- Stay Active: Regular physical activity can strengthen the muscles that support the joints and improve joint function.
- Avoid Joint Injuries: Wearing appropriate protective gear during sports and physical activities can prevent injuries that may lead to joint damage.
- Practice Good Posture: Maintaining proper posture can reduce joint stress and prevent alignment issues that contribute to cartilage wear.
Conclusion
Osteoarthritis is a common degenerative joint disease that can significantly impact a person’s quality of life. Although there is no cure for osteoarthritis, a combination of medical treatments, physical therapy, lifestyle changes, and preventive measures can help individuals manage their symptoms, reduce pain, and improve joint function. Early diagnosis and intervention are key to preventing further joint damage and maintaining mobility. By adopting a healthy lifestyle and working closely with healthcare professionals, individuals with osteoarthritis can lead active, pain-free lives.
References:
- Arthritis Foundation. (n.d.). Osteoarthritis. Retrieved from Arthritis Foundation Website
- Mayo Clinic. (n.d.). Osteoarthritis: Symptoms and Causes. Retrieved from Mayo Clinic Website
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (n.d.). Osteoarthritis. Retrieved from NIH Website