Understanding Monkeypox: Causes, Symptoms, and Treatment Solutions
Monkeypox, a viral infection once considered rare, has recently gained global attention due to outbreaks in various countries. Although it shares some similarities with smallpox, monkeypox is generally less severe. This article explores the causes, symptoms, and effective treatments for monkeypox, providing essential information to help individuals stay informed and protected.
What is Monkeypox?
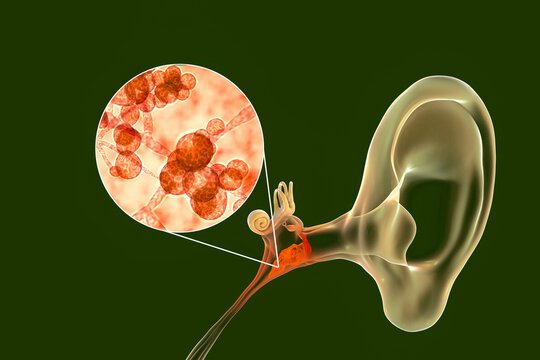
Monkeypox is a zoonotic disease caused by the monkeypox virus, which belongs to the same family as smallpox (Orthopoxvirus). Initially discovered in monkeys in 1958, the virus is transmitted from animals to humans, but recent outbreaks suggest human-to-human transmission is also a growing concern. While the disease is endemic in certain African countries, outbreaks have occurred globally, raising awareness about prevention and treatment.
Causes and Transmission of Monkeypox
Monkeypox is primarily transmitted through contact with infected animals, such as rodents or primates. The virus can enter the body through broken skin, respiratory droplets, or mucous membranes (eyes, nose, or mouth). However, recent cases have demonstrated human-to-human transmission through close contact, including:
- Direct contact with lesions or bodily fluids: The virus can spread when individuals touch an infected person’s skin lesions or come into contact with their fluids.
- Respiratory droplets: Prolonged face-to-face exposure to an infected person can spread the virus via respiratory droplets.
- Contaminated objects: Objects like bedding or clothing that have been in contact with an infected person may harbor the virus, leading to indirect transmission.
- Animal-to-human contact: Handling or consuming infected animals, particularly in regions where monkeypox is endemic, increases the risk of transmission.
Symptoms of Monkeypox
The incubation period of monkeypox is typically 6 to 13 days, but it can range from 5 to 21 days. Symptoms appear in two stages, starting with general flu-like signs and progressing to the characteristic rash.

- Initial symptoms (prodromal phase):
- Fever
- Headache
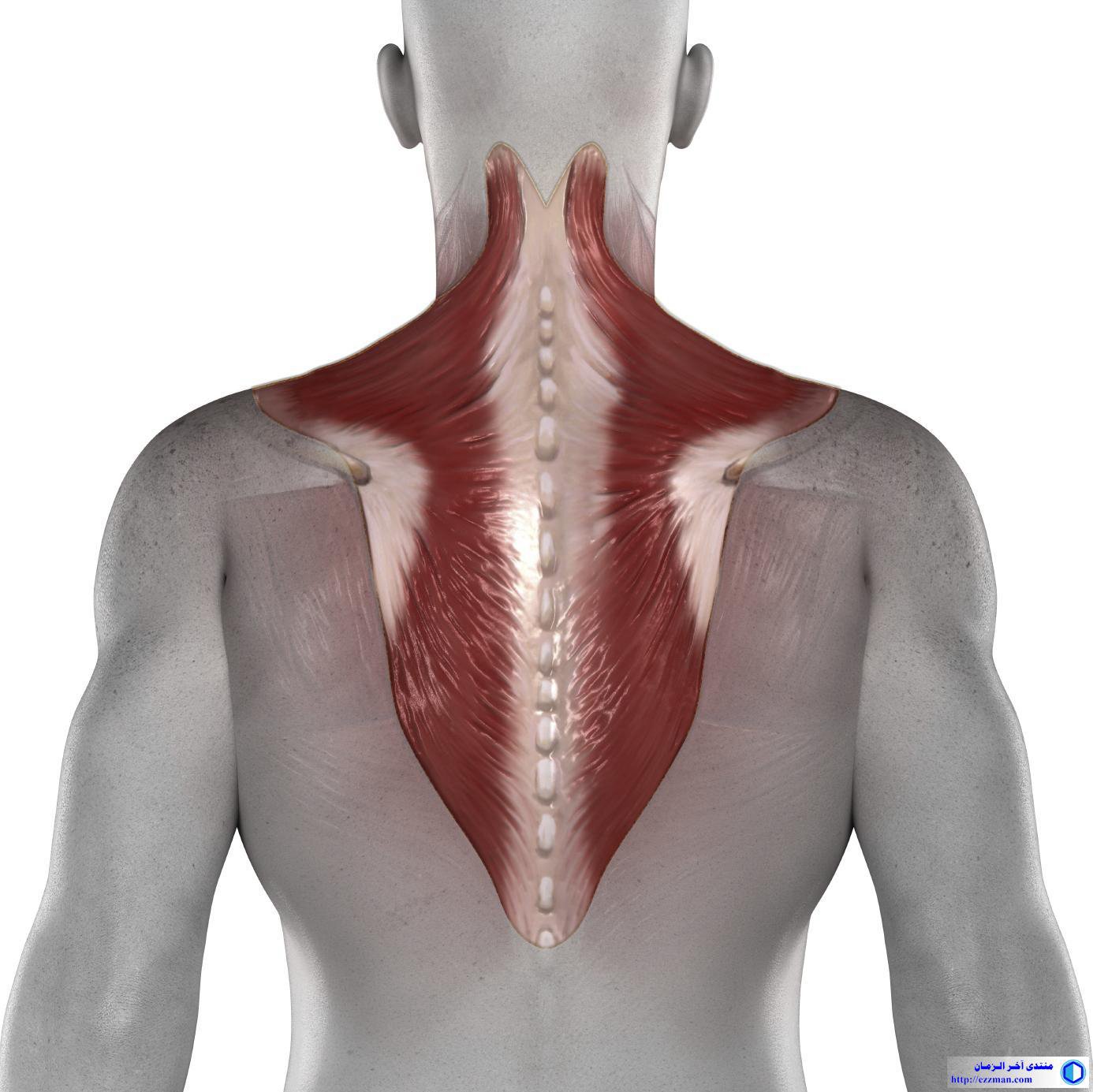
- Muscle aches
- Fatigue
- Swollen lymph nodes (a key difference from smallpox)
- Rash development (secondary phase):
- A rash typically begins on the face and spreads to other parts of the body, including the hands, feet, and genitals.
- The rash progresses through stages: macules, papules, vesicles, pustules, and finally scabs, which eventually fall off.
- The rash is often accompanied by severe itching and discomfort.

Monkeypox is typically a self-limiting disease, with symptoms lasting 2 to 4 weeks. However, severe cases can occur, especially in immunocompromised individuals, pregnant women, and children.
Diagnosing Monkeypox
Accurate diagnosis is crucial for containing outbreaks and preventing further spread. Healthcare providers diagnose monkeypox based on the following:
- Clinical evaluation: Doctors assess symptoms and examine the characteristic rash.
- Laboratory tests: Confirmation is obtained through polymerase chain reaction (PCR) testing of skin lesions or bodily fluids.
- Differential diagnosis: Since the rash may resemble other illnesses such as chickenpox or measles, additional testing may be necessary to rule out these conditions.
Treatment Options for Monkeypox
Currently, there is no specific antiviral treatment for monkeypox. However, the disease’s symptoms can be managed, and several approaches are used to mitigate its effects:
- Supportive care: Treatment primarily focuses on relieving symptoms, including fever management, adequate hydration, and pain relief for those experiencing discomfort from the rash.
- Antiviral medications: In severe cases, antiviral drugs like tecovirimat (TPOXX) have been approved to treat monkeypox. While originally developed for smallpox, these antivirals show promise in reducing the severity of monkeypox symptoms.
- Vaccination: Vaccination against smallpox has been found to provide some protection against monkeypox. The JYNNEOS vaccine (also known as Imvamune or Imvanex) is now recommended for individuals at high risk of exposure, such as healthcare workers and those in contact with infected persons.
- Isolation and infection control: Patients diagnosed with monkeypox should be isolated to prevent transmission. Healthcare providers must follow strict infection control protocols to avoid the spread of the virus.
Preventing Monkeypox
Prevention plays a key role in controlling monkeypox outbreaks. By taking simple precautions, individuals can reduce their risk of infection:
- Avoid contact with animals: In regions where monkeypox is endemic, avoid direct contact with wild animals or eating bushmeat.
- Practice good hygiene: Regular hand washing and using hand sanitizers can reduce the risk of infection.
- Safe handling of contaminated materials: Avoid sharing bedding, towels, or clothing with infected individuals, and ensure proper disinfection of such items.
- Get vaccinated: For those in high-risk groups, vaccination offers an effective way to prevent monkeypox and minimize symptoms in case of exposure.
Conclusion
Monkeypox, though not as deadly as smallpox, still poses a serious health risk, especially with the potential for global spread. Understanding its causes, symptoms, and treatment options is essential for minimizing outbreaks and protecting public health. With appropriate medical care, antiviral treatments, and preventive measures like vaccination, it is possible to manage and control monkeypox effectively.
References
- Centers for Disease Control and Prevention (CDC). “Monkeypox: Signs and Symptoms.” Available at: https://www.cdc.gov/poxvirus/monkeypox/symptoms.html
- World Health Organization (WHO). “Monkeypox: Key Facts.” Available at: https://www.who.int/news-room/fact-sheets/detail/monkeypox
- National Institutes of Health (NIH). “Tecovirimat for Treatment of Human Monkeypox.” Available at: https://clinicaltrials.gov/ct2/show/NCT05534572
This comprehensive guide to monkeypox offers a clear understanding of the disease and emphasizes the importance of treatment and prevention for public safety.