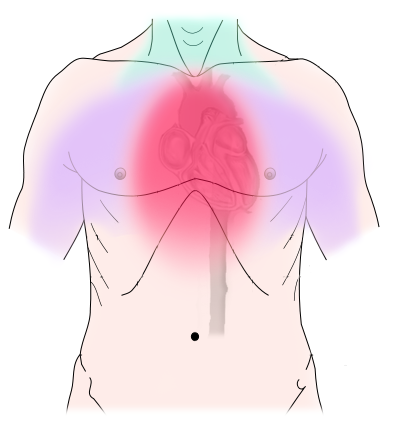
Angina, also known as chest pain or discomfort, is a condition that occurs when the heart muscle doesn’t get enough oxygen-rich blood. This is often a sign of an underlying heart condition and can be a precursor to more severe cardiac events, such as a heart attack. Understanding the different types of angina is crucial for proper diagnosis, treatment, and prevention.
In this article, we’ll explore the various types of angina, their causes, symptoms, and treatment options, so you can take proactive steps to manage your heart health effectively.
What is Angina?
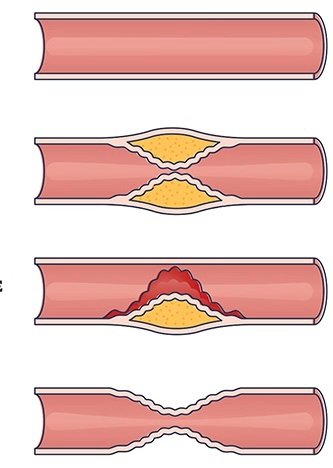
Angina is not a disease in itself but a symptom of coronary artery disease (CAD). CAD occurs when the arteries that supply blood to the heart become narrowed or blocked due to the buildup of fatty deposits called plaques. This restricts blood flow, especially during physical exertion or emotional stress, causing chest pain or discomfort.
The primary types of angina are:
- Stable Angina
- Unstable Angina
- Variant (Prinzmetal’s) Angina
- Microvascular Angina
Each type of angina has different triggers, symptoms, and treatment approaches.
1. Stable Angina: The Most Common Form
Stable angina is the most common form of this condition. It usually occurs during physical exertion or stress, as these increase the heart’s demand for oxygen-rich blood. The arteries, already narrowed by plaque, struggle to deliver enough blood, causing discomfort.
Symptoms of Stable Angina:
- Predictable chest pain that occurs during exertion or stress
- The pain typically lasts for a few minutes and goes away with rest or medication
- Discomfort can radiate to the arms, neck, jaw, or back
Causes:
Stable angina is primarily caused by coronary artery disease. It occurs when the arteries are narrowed by plaque buildup, restricting blood flow to the heart.
Treatment:
Stable angina can often be managed with lifestyle changes and medication. Common treatments include:
- Nitrates: Medications like nitroglycerin are used to widen blood vessels and reduce chest pain.
- Beta-blockers: These reduce the heart’s workload by slowing down the heart rate.
- Calcium channel blockers: These help relax and widen blood vessels, improving blood flow.
- Lifestyle changes: This includes quitting smoking, eating a heart-healthy diet, and regular exercise.
If lifestyle changes and medications are not sufficient, procedures like angioplasty or coronary artery bypass surgery may be necessary to improve blood flow to the heart.
2. Unstable Angina: A Medical Emergency
Unstable angina is a more dangerous condition and is considered a medical emergency. Unlike stable angina, it can occur suddenly and without warning, even at rest. Unstable angina suggests that a heart attack may occur soon.
Symptoms of Unstable Angina:
- Severe and unpredictable chest pain that occurs at rest or with minimal exertion
- Pain that lasts longer than stable angina, typically more than 15-20 minutes
- Pain that doesn’t go away with rest or nitroglycerin
Causes:
Unstable angina is typically caused by a rupture of plaque within the coronary arteries, which leads to the formation of a blood clot. This can block the artery partially or entirely, cutting off blood flow to the heart and increasing the risk of a heart attack.
Treatment:
Unstable angina requires immediate medical attention. The treatment approach includes:
- Medications: These include antiplatelet agents like aspirin, blood thinners (such as heparin), and nitrates to improve blood flow and prevent clotting.
- Hospitalization: Most patients with unstable angina are admitted to the hospital for close monitoring and additional treatment.
- Angioplasty or Bypass Surgery: In more severe cases, doctors may recommend procedures to open or bypass the blocked arteries.
Prompt treatment is essential to prevent a heart attack and to improve long-term outcomes.
3. Variant (Prinzmetal’s) Angina: Caused by Artery Spasms
Variant angina, also known as Prinzmetal’s angina, is a rare type of chest pain caused by a temporary spasm in one of the coronary arteries. These spasms reduce blood flow to the heart, resulting in chest pain.
Symptoms of Variant Angina:
- Chest pain typically occurs at rest, often between midnight and early morning
- Pain can be severe and may last longer than stable angina
- Discomfort may occur in cycles, with multiple episodes in a short time frame
Causes:
Unlike other types of angina, variant angina is not caused by plaque buildup but by a spasm in the coronary artery. These spasms can occur in people with or without coronary artery disease. The exact cause of these spasms is not well understood, but triggers may include:
- Cold exposure
- Stress
- Certain medications
- Smoking
- Use of stimulants like cocaine
Treatment:
The treatment for variant angina typically focuses on preventing and relieving artery spasms. Common treatments include:
- Calcium channel blockers: These medications help prevent spasms by relaxing the blood vessels.
- Nitrates: Nitroglycerin can be used to relieve spasms and ease chest pain.
- Lifestyle changes: Patients are often advised to avoid smoking, stress, and other triggers that may cause spasms.
While variant angina can be controlled with medication, patients are at risk for more serious complications if left untreated.
4. Microvascular Angina: Affects the Small Vessels
Microvascular angina is a less common type of chest pain that affects the heart’s tiny blood vessels rather than the larger coronary arteries. It is sometimes referred to as cardiac syndrome X.
Symptoms of Microvascular Angina:
- Chest pain or discomfort that can last longer than other types of angina
- Pain that is more intense or prolonged than stable angina
- Pain that may not be relieved by rest or medication
Causes:
The exact cause of microvascular angina is not well understood. It’s thought to be related to problems with the small blood vessels of the heart that do not dilate properly, restricting blood flow.
This type of angina is more common in women, particularly after menopause, and is associated with risk factors like high blood pressure and diabetes.
Treatment:
The treatment for microvascular angina is similar to other types of angina and focuses on improving blood flow and reducing symptoms. It may include:
- Medications: Such as nitrates, beta-blockers, and calcium channel blockers.
- Lifestyle changes: Such as eating a heart-healthy diet, exercising regularly, and managing conditions like high blood pressure and diabetes.
Because microvascular angina is less well understood than other types of angina, patients may require specialized care and monitoring.
Managing Angina: A Holistic Approach
Managing angina involves more than just taking medications. Patients are encouraged to make lifestyle changes that support heart health, including:
- Healthy Diet: Eating a diet low in saturated fats, trans fats, and cholesterol can help reduce the risk of angina. Focus on foods rich in fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: Physical activity improves circulation and strengthens the heart. Patients should aim for at least 30 minutes of moderate exercise most days of the week, with approval from their doctor.
- Smoking Cessation: Smoking is a major risk factor for angina and heart disease. Quitting smoking can significantly reduce the risk of further complications.
- Stress Management: High levels of stress can trigger angina. Practices such as meditation, yoga, and deep breathing exercises can help manage stress levels.
Conclusion: Take Charge of Your Heart Health
Understanding the different types of angina is the first step in managing your heart health. Whether you have stable angina that occurs with exertion or a more severe form like unstable angina, knowing the warning signs and seeking timely treatment can prevent serious complications like heart attack.
By adopting a heart-healthy lifestyle, staying on top of medications, and working closely with your healthcare provider, you can effectively manage angina and improve your overall quality of life.
References:
- American Heart Association (AHA): Angina Types and Symptoms
- Mayo Clinic: Angina Overview
- Johns Hopkins Medicine: Managing Angina